- Visiting Hours: Mon-Sat / 8:00 AM - 8:00 PM
- Visiting Hours: Mon-Sat / 8:00 AM - 8:00 PM
- +91 80565 80565 / 044 46878787
Dr SM Rajendran has more than 40 years of experience. He completed his MBBS (1970) and MD (1978) from the University of Madras, and his Doctor of Science (DSc.) in 2012. He taught Internal Medicine and Diabetology at Stanley Medical College and served as Director and Professor of Diabetology at the Sree Balaji Diabetology Research Center, Chennai.
Mon – Sat / 9:00 AM to 1:00 PM
The first step to treating any disease is finding out if the individual has it in the first place, and if they do, what is the severity and progression of the illness. For diabetes, an early diagnosis and intervention can help minimize the long-term adverse effects and symptoms associated with the disease.
Before devising a treatment plan for this disease, it is essential to identify whether the person has Type 1 or Type 2 diabetes. The signs and symptoms and the age of onset vary between the two subtypes.
In Type 1 diabetes, the symptoms are seen at a young age (usually in adolescence or teens, generally less than 25 years). With Type 2 diabetes, typically, adult onset is observed, and symptoms start appearing during middle age. Some of the common symptoms across Type 1 and Type 2 diabetes are:





There are several non-invasive and invasive tests for diabetes. Blood tests are typically done for the diagnosis and monitoring of a person with diabetes. The blood test involves pricking a finger for analysis of the blood drop or the collection of a blood sample via syringe to check the blood sugar levels.
The diagnosis for diabetes often involves a test for glycated haemoglobin (HbA1c). Urine sample analysis may be done as a non-invasive test to check for sugar and ketone bodies in the urine. The urine test can help the medical professional get a clear idea of the disease severity and assess if the kidneys have been affected.
Apart from these, certain blood serum tests for immune markers are done to confirm if the individual has Type 1 diabetes. In Type 1 diabetes, the body’s immune system attacks the cells that produce insulin, leaving behind molecular fingerprints of this self-destructive action. The immune marker tests track this evidence to assess the extent of damage the disease has caused and the duration since its onset.
The typical tests done for a person having or suspected of having diabetes are:



The primary method of diagnosing and monitoring diabetes is the HbA1C test. When the blood sugar levels are high for a prolonged period, some of that glucose is absorbed by the haemoglobin (the oxygen-carrying part) in the circulating red blood cells. This count is a good indicator of how much and for how long the person’s blood sugar has been high.
The higher your blood sugar levels, the higher the levels of haemoglobin with sugar attached. An HbA1C level of 6.5% or higher on two separate tests means the individual has diabetes. An HbA1C between 5.7% and 6.4% indicates prediabetes, and a level below 5.7% is considered normal. This test does not require fasting, as it measures the evidence of high sugar levels over a long time.






This test can be taken anytime before or after food and does not require fasting. Regardless of the meal timing or the specific food eaten before the test, a random blood sugar level of 200 mg/dL or more is indicative of diabetes. Doctors usually take this test as a first step, when the patient has just eaten or is not sure of when their last meal was. A random blood sugar test is followed up with other tests before a diagnosis of diabetes or prediabetes is confirmed, as certain environmental conditions such as dehydration or strenuous exercise can lead to inaccurate results.
This test is taken after a night of fasting (the last meal should be had 10-12 hours before) and with limited fluid intake. The individual will be asked to take an early meal and a limited amount of water before the test so that the results are not altered artificially.
If you have a fasting blood sugar level of less than 90 mg/dL, it is normal. A fasting blood sugar level of 90 to 125 mg/dL (5.6 to 6.9 mmol/L) is considered prediabetes. If the value is 126 mg/dL or higher on two separate tests, the individual is considered to be diabetic.
For this test, you are required to fast the whole night, then a fixed amount of glucose is given orally. The sugar levels are checked one hour later. This test is done mainly for pregnant women, women who are older than 35 years and pregnant, and women with a history of diabetes during pregnancy. The test measures the body’s capacity to process insulin on an empty stomach and clearly identifies insulin resistance. This test is not used for Type 1 diabetes.








Prevention is always better than cure. We perform routine physical and wellness check-ups to ensure that any disease is detected and treated in its initial stages.



The treatment for diabetes comprises healthy food habits, lifestyle changes, exercise and prescribed medication. For a diabetic person, an effective treatment plan will include all of the above. If their blood sugar levels are brought under control, the medication may be reduced. Maintaining a proper diet and physical activity alongside can keep the blood sugar under control for a long time. (Referred to as a remission)
One of the key factors that increase the risk of getting diabetes earlier is an unbalanced diet high in food items with processed sugar, oil and fat, such as soft drinks, fried items and fast food. If you have diabetes or prediabetes, you must drastically reduce or halt your sugar intake. The food quantity per meal should also be reduced. Timely meals in limited quantities with low/ no sugar can help maintain the sugar levels and even lead to a remission in diabetes. Both young and old people should adhere to a diet plan for the best results.



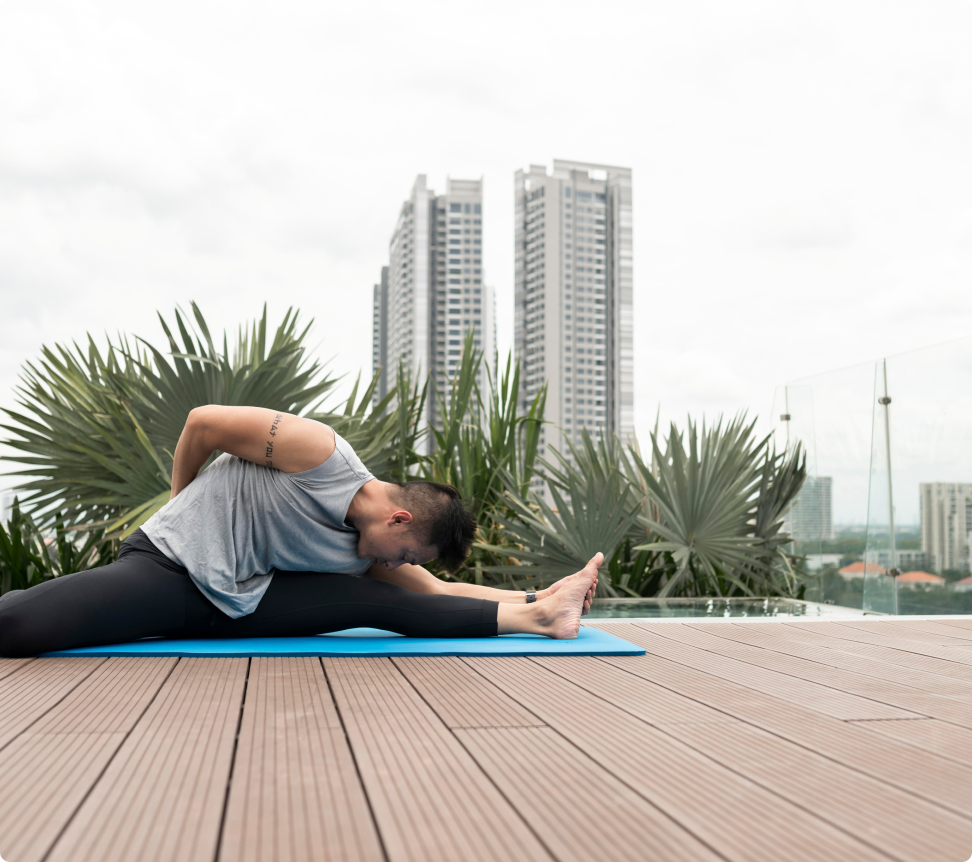
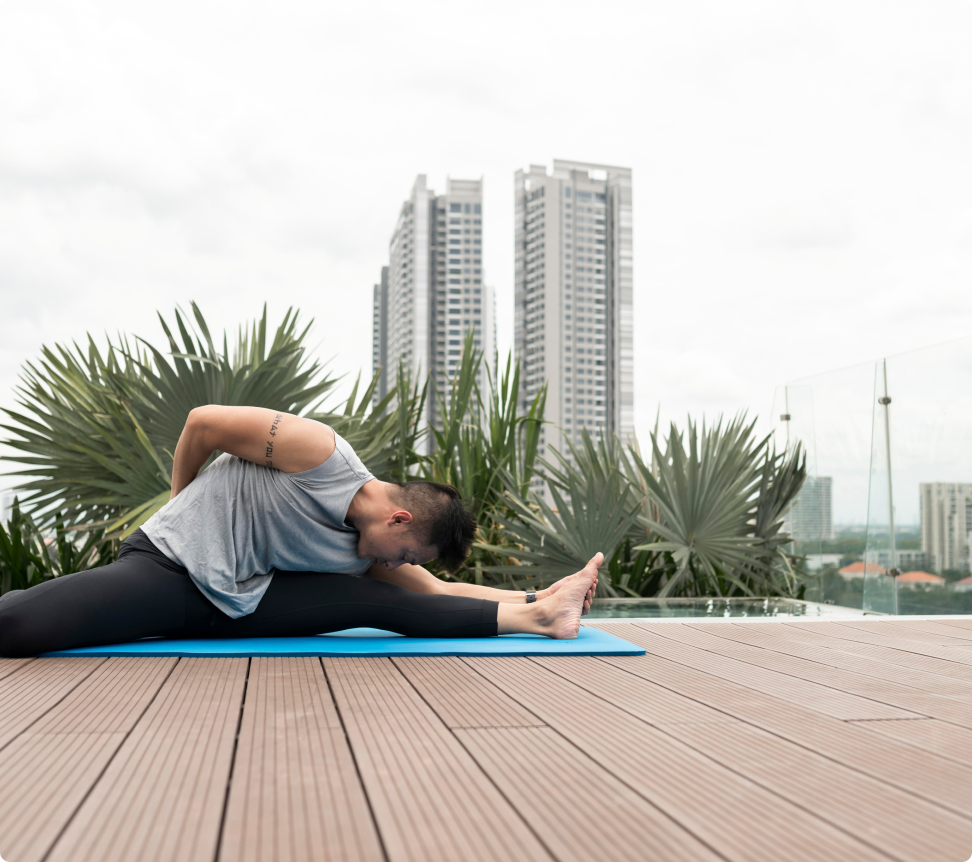
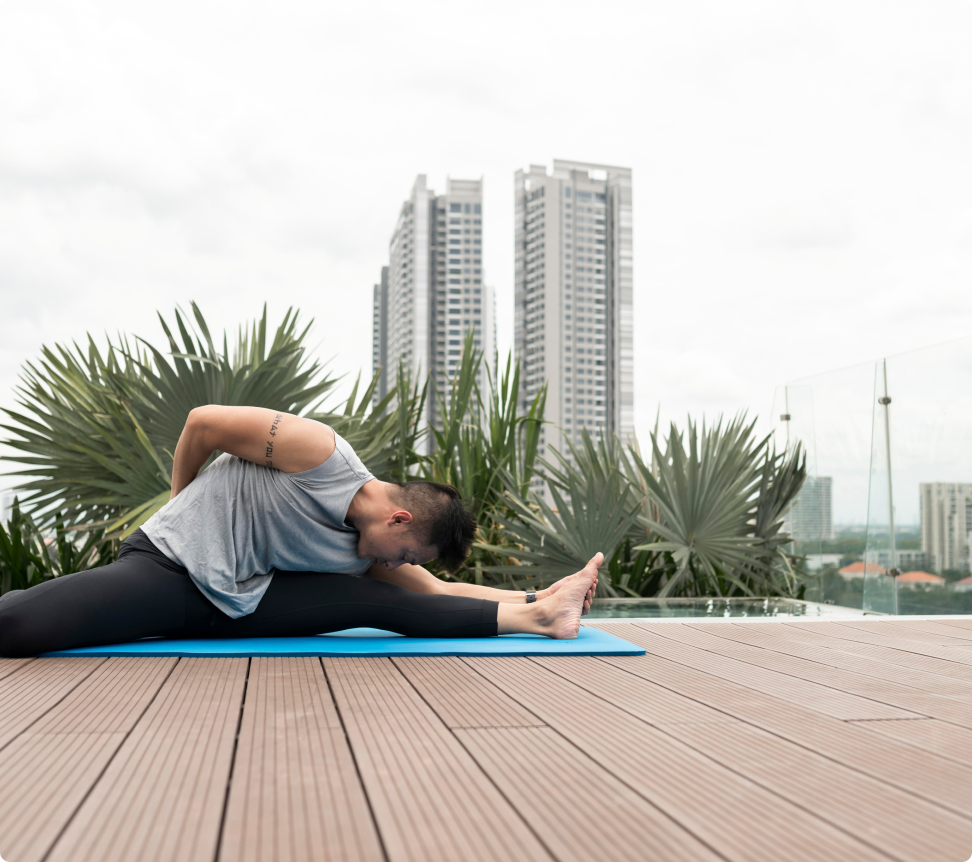
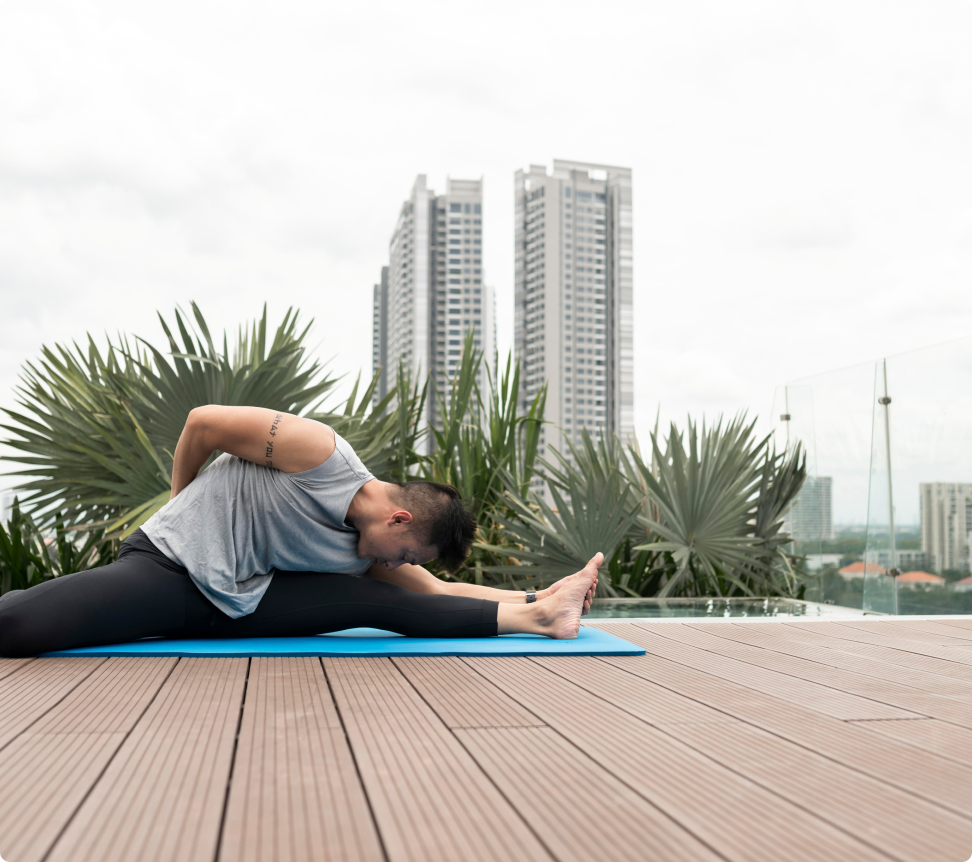
All of us need exercise to keep our bones, muscles and metabolism healthy. A lack of exercise and a sedentary lifestyle can lead to increased weight gain, stress on vital organs, fat build-up in the liver, etc. In young people, regular outdoor exercises like walking, jogging, cycling and running can help regulate blood sugar levels and keep their weight at the optimum level. Outdoor exercise should be preferred over indoor exercise to reduce the need for high doses of medication as part of diabetes treatment.
Diabetes is often called a ‘lifestyle disease’. Some recommended lifestyle changes to control or prevent it are:


The mainstay treatment for diabetes is replacing the insulin the body can no longer produce, along with other medicines to help reduce the blood sugar level and increase sugar storage in cells. This requires taking insulin injections periodically along with tablets. The treatment is adjusted based on regular tests for blood sugar level, and dosages increased or decreased accordingly.
Type 1 diabetes requires lifelong treatment even with a good lifestyle and adequate exercise, as the body is unable to produce insulin, and an external supply through injection or pump would be constantly required.
The treatment for Type 2 diabetes is multi-pronged and involves the following:
Diet and exercise go hand in hand for treating diabetes and involve cutting down on carbohydrates and fatty foods, taking up cardio and resistance exercises, eating at regular times and getting adequate rest. Following these steps usually leads to weight loss. Doctors advise patients to get their weight within the acceptable BMI limits (19-25) so that it doesn’t exacerbate the condition of diabetes.
Regular blood monitoring helps to decide if a further course of treatment is necessary. Individuals with high blood sugar despite these steps are prescribed medication, sometimes along with insulin. With the correct lifestyle changes, Type 2 diabetes can go into remission and may not require medicines. It’s important to note that medication can have side effects such as nausea, vomiting, bloating, dysentery, etc.




The treatment for gestational diabetes (gestational diabetes mellitus or GDM) usually involves the following:
Women with a high BMI, abnormal weight gain and aged over 35 are at risk of developing insulin resistance and diabetes during their pregnancy. So, regular sugar monitoring via OGCT tests (every 3 months) is mandatory. If the levels are high, medicines are required, and in some cases, insulin injections may be prescribed. Individuals with GDM are monitored throughout their pregnancy and a few months after delivery.
An important part of the treatment plan is close monitoring of the baby’s health with regular ultrasound scans to ensure development is normal. GDM can lead to the mother developing Type 2 diabetes after the baby is born, so monitoring the mother after delivery (for 6-12 weeks) is also vital.


A person with prediabetes is on the cusp of developing the disease but does not have it yet. So, the treatment focuses on preventive measures to ensure they do not get the disease.
Doctors recommend the following measures for prediabetic individuals:
People with prediabetes usually have one or more risk factors that are affecting their health and bringing on an onset of the disease. Following the above steps, along with regular checkups, can keep their health stable for decades.





Oral medication is part of the treatment plan for Type 2 diabetes primarily. Insulin is as yet not available in tablet form (it gets digested in the stomach and intestines) and thus cannot be given orally for Type 1 diabetes. Oral medicines can be of several types:
The medicine dosage and frequency is decided based on the severity of the disease.
Insulin is the primary line of treatment for diabetes, especially Type 1. Currently, it is administered as an injection or via insulin pumps (more expensive but reduces need for pricking). There are no insulin tablets or pills, as it gets broken down in the stomach before it can be used by the body. Some types of insulin medication are:



Would you like to manage your diabetes better and lead a healthier, normal life?
Take an appointment with our senior diabetologist today!


No 6, 6th Main Road, Opp. Indian Bank. Nanganallur, Chennai - 600061
+91 80565 80565 / 044 46878787
contact@dihaclinic.org
Mon - Sat / 8:00 AM - 8:00 PM
 Vishnu Rajan2024-06-03Highly recommended for the services provided here; Excellent ambience; clean and hygienic area where the medical procedures are performed; kind medical and non-medically staffs; Bonus points for the kids-area. Keep up the good work.
Vishnu Rajan2024-06-03Highly recommended for the services provided here; Excellent ambience; clean and hygienic area where the medical procedures are performed; kind medical and non-medically staffs; Bonus points for the kids-area. Keep up the good work. Gopalachari Ramarajan2024-05-31Sir Madam I am very much happy about the hospital check up to my highest satifasfaction Staffs doctors very much responsive well attending needs to the patients more over hospital are well maintained neat n clean the rates for the tests are not high compare to other hospitals.
Gopalachari Ramarajan2024-05-31Sir Madam I am very much happy about the hospital check up to my highest satifasfaction Staffs doctors very much responsive well attending needs to the patients more over hospital are well maintained neat n clean the rates for the tests are not high compare to other hospitals. dharmarajan viswanathan2024-05-25We had a good consultation and advice from Dr.Rajendran. His patient hearing and observation from the file really good. He creates confidence that is what most doctors now don't do it. His approach is so nice. We will recommend this doctor and clinic
dharmarajan viswanathan2024-05-25We had a good consultation and advice from Dr.Rajendran. His patient hearing and observation from the file really good. He creates confidence that is what most doctors now don't do it. His approach is so nice. We will recommend this doctor and clinic Natarajan Subramanian2024-05-16I recently had the pleasure of visiting Sudha ma'am at Diha clinic for my thyroid concerns. From the moment I walked in, the atmosphere was warm and welcoming, which immediately put me at ease. The staff was friendly and efficient, making the entire process seamless. Sudha maam was excellent and she took the time to listen to my concerns and answer all of my questions, never making me feel rushed. Thanks to Dr. Sudha Balasubramnian's guidance and treatment plan, I've seen significant improvements in my thyroid health. Overall, my experience at Diha was exceptional
Natarajan Subramanian2024-05-16I recently had the pleasure of visiting Sudha ma'am at Diha clinic for my thyroid concerns. From the moment I walked in, the atmosphere was warm and welcoming, which immediately put me at ease. The staff was friendly and efficient, making the entire process seamless. Sudha maam was excellent and she took the time to listen to my concerns and answer all of my questions, never making me feel rushed. Thanks to Dr. Sudha Balasubramnian's guidance and treatment plan, I've seen significant improvements in my thyroid health. Overall, my experience at Diha was exceptional Lakshminarasimhan lanhan2024-05-15It is a well maintained clinic with expert doctors in all faculties. The NABL attached pathological lab is managed well by experts in the field. The ambience adds a feel good factor that is sure too assure the patients to get well. The pharmacy attached dispenses all medicines and the patients need not run hither and thither. The front-office personnel are very receptive and assist the patient in the best way they can. Systems are in place, therefore, the prescriptions given are all neatly printed. I pray good health for all through their life, but we are bound to get sick and if such a situation befalls, you can just walk into Diha clinic at Nanganallur for treatment. Stay blessed Stay healthy. Kudos to Team Diha Clinic, Nanganallur, Chennai -600061
Lakshminarasimhan lanhan2024-05-15It is a well maintained clinic with expert doctors in all faculties. The NABL attached pathological lab is managed well by experts in the field. The ambience adds a feel good factor that is sure too assure the patients to get well. The pharmacy attached dispenses all medicines and the patients need not run hither and thither. The front-office personnel are very receptive and assist the patient in the best way they can. Systems are in place, therefore, the prescriptions given are all neatly printed. I pray good health for all through their life, but we are bound to get sick and if such a situation befalls, you can just walk into Diha clinic at Nanganallur for treatment. Stay blessed Stay healthy. Kudos to Team Diha Clinic, Nanganallur, Chennai -600061 Nalini R2024-04-27Dr Sudha is such a friendly person and listens to our problems with patience. Hospital staffs are very polite and easily approachable. Ambience is very good and the rest rooms are maintained in a very hygienic manner. I would recommend Diha clinic for any health concerns.
Nalini R2024-04-27Dr Sudha is such a friendly person and listens to our problems with patience. Hospital staffs are very polite and easily approachable. Ambience is very good and the rest rooms are maintained in a very hygienic manner. I would recommend Diha clinic for any health concerns. google user2024-04-27Excellent facilities, very neatly maintained, and the doctors and clinic staff are very kind and helpful.
google user2024-04-27Excellent facilities, very neatly maintained, and the doctors and clinic staff are very kind and helpful. Balan L S2024-04-22Consulted Dr Niranjanan and his approach, consult and describing medicines are very suitable to us. We are just satisfied with the service of Diha Clinic.
Balan L S2024-04-22Consulted Dr Niranjanan and his approach, consult and describing medicines are very suitable to us. We are just satisfied with the service of Diha Clinic.
No 6, 6th Main Road, Opp.Indian Bank. Nanganallur, Chennai - 600061
Copyright © 2024 Diha Clinic. All rights reserved | Designed by Spidergems